What is Australian flu? How to prevent the virus and the symptoms to look out for

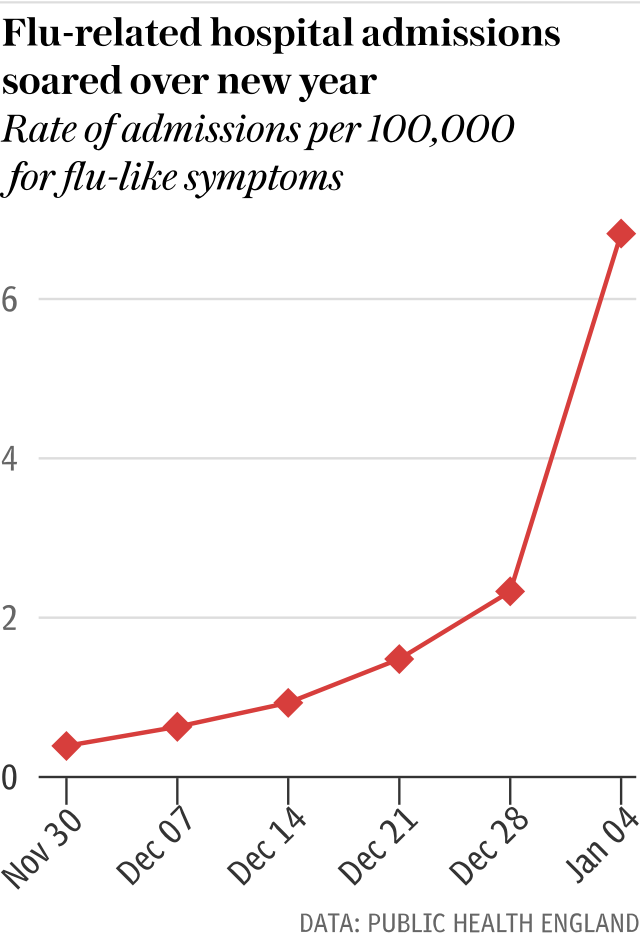
The number of flu-related hospital admissions has tripled in a week, with one in four of those patients suffering from the deadliest strain, Australian flu.
The latest statistics suggest around 4.5 milllion people in England are suffering "influenza-like symptoms".
Last week, 24 people died from flu in the UK. According to Public Health England, the total number of those with flu in hospital has risen from 1,280 to 3,750 in a week, a 2.9-fold rise.
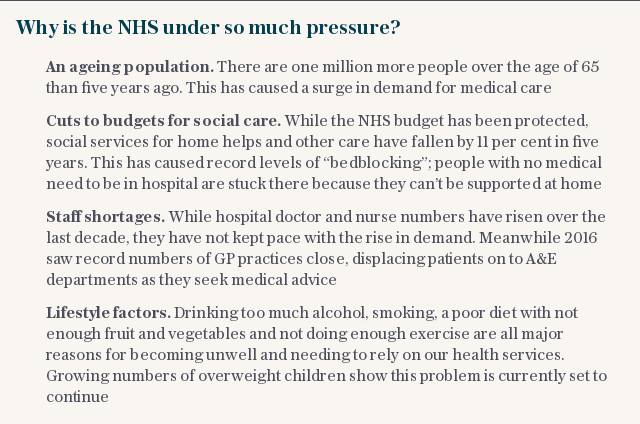
The arrival of Australian flu - also known as Aussie flu - comes amid a winter crisis in the health service. NHS England has urged hospitals to defer planned operations and routine outpatient appointments until the end of the month.
The strain is of particular concern due to fears that current vaccinations are not providing effective protection to the elderly.
In recent years, the NHS has seen increasingly long waits over winter, with some of the worst waiting times on record last winter.
However, for almost a decade the NHS has escaped a heavy flu season, with the last pandemic seen in 2009.
Here is everything you need to know about the virus.
Why is it called Aussie flu?
The influenza virus can change every year, which means the flu you contract this year could be a different type to the one you suffered from last year.
While the official name of the flu circulating the UK this winter is H3N2, it has recently been dubbed Australian - or Aussie - flu. This is because the same strain fuelled the worst flu crisis Australia had experienced for around two decades.
The colloquial names given to different flu strains can be based on:
the year of discovery or isolation
where the flu originated
the strain number
which animal the flu originated from (for example, swine flu)
The particular strain of H3N2 flu that is affecting the UK is similar to the type that Australia suffered from earlier this year, during their winter.
Over 217,000 Australians had confirmed cases of the virus in 2017, over double the previous record of just over 100,000 in 2015.
What are the symptoms?
Dr Richard Pebody, acting head of respiratory diseases at Public Health England, said the H3N2 influenza can cause problems for the elderly - and can particularly result in care home outbreaks.
According to the NHS, the symptoms to look out for in adults include:
a sudden, high fever, with a temperature of 38C or above
aching body
feeling tired or exhausted
dry, chesty cough
diarrhoea or tummy pain
sore throat
nausea and being sick
headache
loss of appetite
difficulty sleeping
Children can also suffer from earache when they have the flu.
Will the flu vaccine help?
Dr Pebody said the flu vaccine is currently the best preventative for flu.
He said that while the effectiveness data for this year's flu is not yet available, he hopes the vaccine will provide "reasonable protection" against Australian flu.
Last year, the vaccine offered protection to two thirds of children and four in ten adults under 65. However, it had almost no effectiveness in pensioners, which has caused concerns. But effectiveness can change from year to year, and officials are urging all those eligible to take up the vaccine.
While it takes 10 to 14 days for the vaccine to take effect, Dr Pebody encouraged those who can take advantage of the NHS's free programme, which includes anyone who is pregnant or over the age of 65, to do so.
Professor Helen Stokes-Lampard, chairman of the Royal College of GPs, said: "The entire NHS is currently facing intense winter pressures and NHS staff in all areas of the service are working incredibly hard to deliver the best care possible for their patients.
"Although we are reaching peak flu season, we want to reassure patients that the influenza vaccine remains the best protection against flu this winter period.
"It is not too late for patients to receive their vaccination, and we would encourage patients, particularly those in an at-risk group, such as those with long-term conditions and pregnant women, to have a flu jab from their GP practice or pharmacist."
When should you go to the hospital?
If you develop a sudden chest pain, have difficulty breathing or start coughing up blood, call 999 or go to A&E.
You should contact your GP if your symptoms don't improve after seven days, you are 65 or over, pregnant, or have a long-term medical condition (such as heart, lung or kidney disease, diabetes or a neurological disease).
You should also speak to your GP if you already have a weakened immune system - for example, due to HIV or chemotherapy.
What about the norovirus?
As well as higher levels of flu, the norovirus is also causing problems for hospitals. Six hospital wards are now on lockdown as outbreaks of norovirus continue to spread across Northumberland and North Tyneside.
The norovirus, which causes diarrhoea and projectile vomiting, is one of the UK's most common stomach bugs.
It is more prevalent in the winter, with levels of the illness contributing to current NHS pressures.
An NHS spokesperson said: "This isn't just one large outbreak - as both flu and norovirus are in the community it will continue to be brought into our hospitals.
"Often this is unavoidable - if the patient is frail or very young for instance - as anyone in need of care will always receive it.
"However, wherever possible we are urging residents to either call 111 or talk to a pharmacist rather than risk bringing either bug into the hospital. Both are nasty but with common sense steps - drinking lots of water and staying warm - they can be managed."
There is no cure for norovirus, meaning the best thing for anyone suffering from norovirus to do is to stay at home and let it run its course.
The Northumbria Healthcare NHS Foundation trust is also recommending that no children under the age of 16 come as a visitor to inpatient wards and hospital facilities due to the on-going flu and norovirus outbreaks.
A spokesperson said: "They will not be allowed to visit maternity, pregnancy assessment or the birthing unit under any circumstances. Only immediate family will be permitted to visit the Special Care Baby Unit.
"This is for both their own and our patient's safety as they are among the most at risk of catching and/ or carrying both flu and norovirus."
They added: "In areas where visiting is open please remain vigilant: wash your hands thoroughly (soap and water - not alcohol gel).
"Please do not visit if you have symptoms of norovirus or any respiratory or flu-like symptoms; you will only endanger yourself, our staff and your loved ones."
