Push to improve syphilis testing in US as disease makes dramatic comeback
Syphilis was until recently an anachronism to medical professionals.
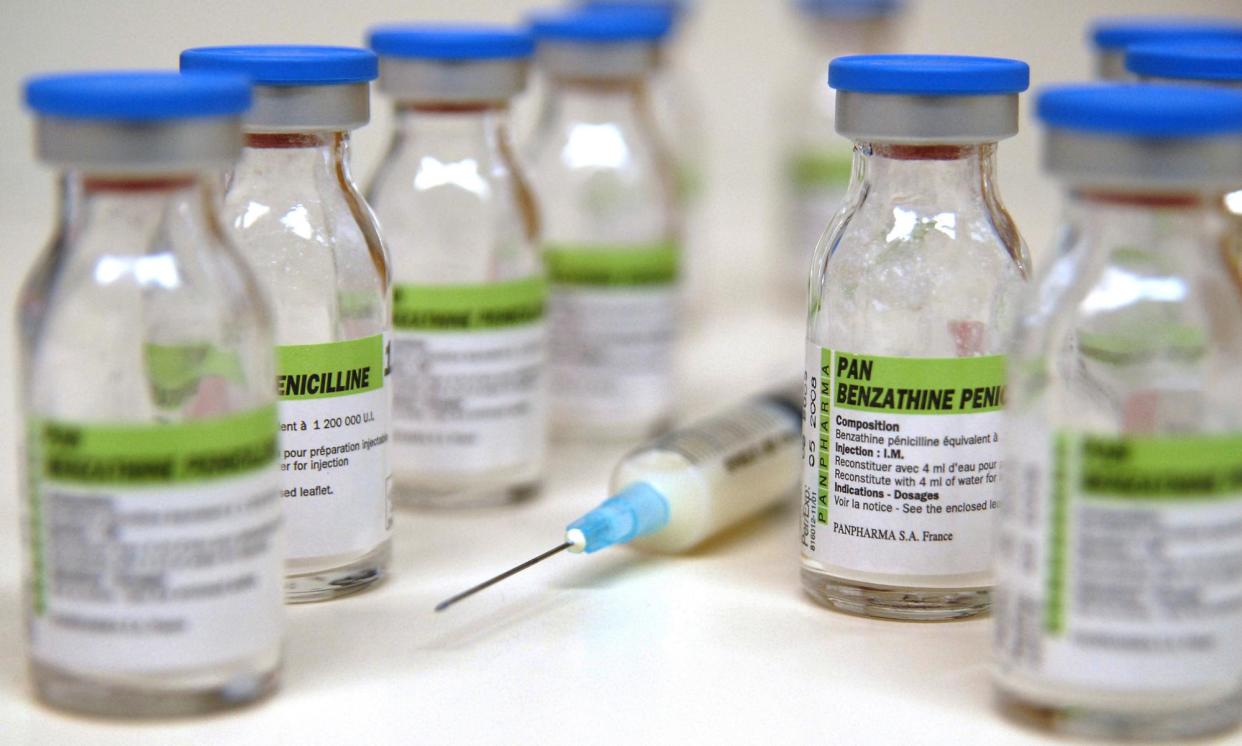
The sexually transmitted infection (STI) was so common in the 19th century that it earned its own specialism – syphilology – but the advent of penicillin in the 20th century meant the disease could be easily treated, and by the 1990s syphilis had been nearly eliminated from the US.
However, over the last decade it has mounted a dramatic comeback. Cases have risen 80% in the last five years, and the US now has the highest syphilis rates since 1950. More than 200,000 Americans were diagnosed with the disease in 2022. Since 2012, the US Centers for Disease Control and Prevention (CDC) has documented a 10-fold increase in the number of babies born with the disease.
Last week, the National Institutes of Health (NIH) took a significant step toward fighting back against one of the key problems – the fact that testing for syphilis is so difficult. It said it will spend $2.4m to advance syphilis testing, which hasn’t changed much since the 1950s, into the 21st century.
David Harvey, executive director of the National Coalition of STD Directors, called the new funding “a testament to the federal syphilis taskforce”, a group convened to address the wave of new cases.
But “combatting an STI like syphilis does not solely relate to improving diagnostics”, he noted, referring to testing. “We need increased diagnostic tools in other areas, and we need increased investments in therapeutic research and vaccines.”
The bacteria that causes the disease, Treponema pallidum, is one of the most invasive known to medicine. T pallidum can cross the blood-brain barrier, the placenta in pregnant mothers and invade any organ system, attacking organs like the heart or bones.
Common symptoms include painless ulcers around the vagina, penis, anus or in the throat; a rash on the hands and feet; flu-like symptoms and patchy hair loss. But these early symptoms are often mild and come and go.
More advanced stages of the disease can bring feared complications, such as neurosyphilis, with dementia-like effects, or ocular syphilis that can cause blindness. Congenital syphilis, when the disease is passed from mother to child, is a special horror: the disease can cause death and neurological devastation in infants.
The disease’s presentations are so varied that one of the father’s of modern medicine remarked: “He who knows syphilis knows medicine.” But both testing and treatment remain stuck in the mid-20th century. Treatment is still highly effective and, bluntly, involves a big shot of penicillin in the rear. But testing is tricky.
“Diagnosis of syphilis is surprisingly challenging and difficult,” said Caroline Cameron, a biochemistry and microbiology professor at the University of Victoria in Canada who was awarded a two-year NIH grant to advance testing to detect the bacteria directly.
The technology still relies on serology, or a test for an immune response. It takes days to weeks for a syphilis diagnosis to be confirmed, and tests cannot determine if an infection is active or cleared. Testing in infants, who lack a fully formed immune system, is especially difficult.
Cameron’s research looks at detecting syphilis proteins using mass spectrometry, a lab tool that measures the ratio of mass to electrical charge for molecules. If successful, the research could solve one of the biggest frustrations of syphilis testing: determining whether an active infection is present.
“What the field needs is something that can directly detect the presence of the pathogen, not the host response to the pathogen, and have it be in that really easy format,” Cameron said. Her lab “is taking patient samples like urine like blood and then analyzing for these proteins that are only found in this pathogen – they’re not found in any other infectious disease, they’re not found in any human protein”.
Serology is “a reasonable approach”, said Dr Stephen Salipante, a professor in the department of laboratory medicine and pathology at the University of Washington, and another NIH grantee. “It’s well vetted, it’s used by lots of clinical laboratories.”
However, with potentially weeks between diagnosis and treatment, “oftentimes the patients can be diagnosed with syphilis but lost to follow-up”, said Salipante. “So you’ve diagnosed the patient but you’ve lost the patient and can’t treat them.”
This has proved especially problematic because of who is at risk for syphilis – most often, marginalized people underserved by medicine. Mothers who give birth to children infected with syphilis provide an especially potent example: 40% lacked prenatal care, but such women only account for about 5% of all pregnant women. Men who have sex with men and people with substance use disorders are also more likely to have syphilis than the general population.
Salipante’s research explores whether researchers can create a test using DNA molecules called aptomers – single-stranded nucleic acid molecules that target specific diseases, such as syphilis. The goal is for such a test to be given at the doctor’s office while the patient waits, perhaps in as simple a format as a dipstick.
“The most important aspect of this is that it is, theoretically, something that can be done very rapidly in a point-of-care setting,” said Salipante. “Instead of sending this to a lab remotely … our ultimate goal and hope is this could be run very rapidly, in 30 minutes or an hour, by nonspecialists in a doctor’s office or emergency room, and could be run while the patient is still there.” Aptomer tests have already been developed for some other infectious diseases, such as Covid-19, though they remain experimental.
Dr Joshua Lieberman, assistant director of the molecular diagnosis and microbiology section also at the University of Washington, is hopeful molecule-specific testing could also help with recurrent antibiotic shortages in syphilis treatment. Lieberman is Salipante’s co-investigator.
The penicillin product used to treat syphilis is Bicillin L-A, an antibiotic that has experienced recurrent shortages driven in part by the explosive growth of syphilis cases. The antibiotic is known to be difficult to produce, and is still derived from mold.
“What I’d like to be able to do is combine that test – yes or no that organism or its DNA is present – with, ‘Is there a marker for resistance to a specific antibiotic in that organism?’” said Lieberman. “This is like what we do with a lot of our testing for mycobacteria in tuberculosis,” he said. This could both help identify antibiotic resistance and susceptibility to new antibiotics.
Harvey noted that even if diagnostic research is successful – and hits the trifecta of good, cheap and quick that researchers seek – the US will still need to invest in STI clinics to deploy the technology.
“You have to have increased research coupled with a robust public health infrastructure,” said Harvey. “That includes public education campaigns and outbreak response.”
